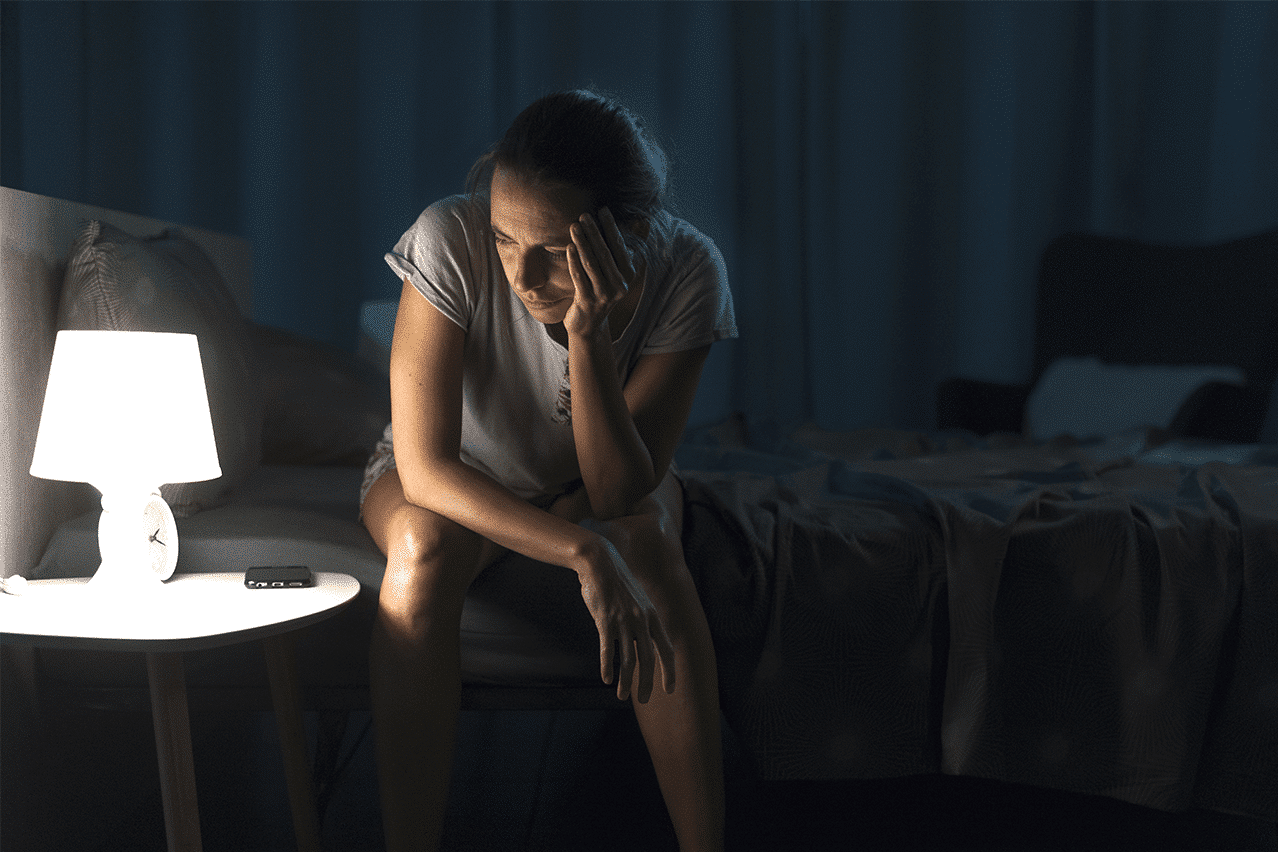
Most people brush off a rough night of sleep. You wake up groggy, power through the day with coffee, and tell yourself you’ll catch up on rest later. But when sleepless nights become the norm instead of the exception, the consequences don’t just show up under your eyes, they show up in your mental health, too.
Insomnia is one of the most underestimated triggers of emotional distress. It creeps in quietly, disrupts your natural rhythm, and slowly chips away at your emotional resilience. What begins as “just a little trouble sleeping” can spiral into something far more serious: chronic anxiety, depression, and even full-blown burnout.
When the Body Doesn’t Sleep, the Mind Doesn’t Heal
Sleep is not just rest, it’s a form of repair. During deep sleep, your brain clears waste, resets neurotransmitters, and processes emotions. Without this essential reset, you’re left operating on fumes.
Insomnia disrupts this process. And when the brain doesn’t get the downtime it needs, emotional regulation begins to suffer. You’re more irritable, less patient, and easily overwhelmed. Tasks that once felt manageable start to feel impossible. Over time, this creates a snowball effect. Your mental capacity shrinks as stress builds.
You can’t pour from an empty cup. And insomnia quietly drains it, drop by drop.
The Anxiety-Insomnia Cycle: A Vicious Loop
One of the most common emotional companions of insomnia is anxiety. And frustratingly, they tend to feed each other in a loop.
You lie in bed worrying about tomorrow’s to-do list. Your mind races. You check the clock; it’s 2:00 AM. The anxiety about not sleeping makes it even harder to fall asleep, and you wake up exhausted. As the cycle repeats, your brain starts associating bedtime with stress.
The more nights you spend tossing and turning, the more anxious you become. It’s a loop that’s tough to break, but it starts with recognizing that insomnia isn’t just a symptom of anxiety; it’s often a driver of it.
Depression: When Sleeplessness Steals Your Joy
Sleep disturbances are a core feature of depression. But insomnia doesn’t just tag along for the ride, it can help drive the condition forward.
People with chronic insomnia are significantly more likely to develop depression. Why? Because sleep deprivation alters brain chemistry, particularly in areas tied to mood regulation like serotonin and dopamine. Over time, this imbalance can drain your energy, numb your emotions, and strip away your ability to feel joy or connection.
The worst part? When you’re depressed and not sleeping, it becomes harder to find the motivation to seek help. You may isolate, withdraw, or assume this is just your “new normal.”
It’s not. And you don’t have to live this way.
Burnout: The Slow Fade Caused by Sleeplessness
Burnout isn’t just about long work hours or high-pressure jobs. At its core, burnout is about depletion of energy, patience, and mental bandwidth. And chronic insomnia is a fast track to that depletion.
You may still be going through the motions, showing up to work, handling responsibilities, but you’re emotionally checked out. The passion you once had is replaced by numbness. Small tasks feel monumental. And because burnout is so often associated with productivity, people ignore the role poor sleep plays in it.
When your brain doesn’t get rest, your body can’t recover. And when you ignore that fatigue, burnout comes knocking.
The Warning Signs You Shouldn’t Ignore
Insomnia often doesn’t come alone. If you’re dealing with consistent sleep disruption, it’s worth paying attention to the following signs:
- Persistent low mood or irritability
- Racing thoughts or constant worry
- Difficulty concentrating or remembering things
- A sense of emotional numbness or detachment
- Physical symptoms like headaches, muscle tension, or digestive issues
- A loss of interest in things you once enjoyed
These aren’t just signs of a bad week. They’re signs that something deeper is going on, and that support might be needed.
What You Can Do
The good news is that insomnia isn’t a life sentence. It’s treatable, and addressing it can have a profound effect on your mental health.
A few approaches that help:
- Cognitive Behavioral Therapy for Insomnia (CBT-I): One of the most effective treatments that addresses both sleep habits and thought patterns.
- Sleep hygiene improvements: Consistent bedtimes, reduced screen time, and winding down rituals make a difference.
- Stress-reduction practices: Mindfulness, gentle exercise, and breathing techniques can ease both anxiety and sleep disruption.
- Professional support: Sometimes, sleep issues are tied to deeper emotional concerns. A therapist can help untangle the root causes and provide tailored solutions.
In Closing
Insomnia might seem like a background issue, just something to deal with on top of everything else. But the truth is, it’s often the silent engine behind much deeper struggles with anxiety, depression, and burnout.
If you’ve been running on empty, consider this your reminder: your mental health is worth the rest. You deserve nights of deep sleep and days full of energy. And with the right support, healing is possible.
Let your rest become a priority again. Your mind will thank you for it.
Theta Burst TMS Therapy for Depression Relief
Top 3 Neuro Navigated TMS FAQs & SmartFocus Guide
Best 2 MeRT Therapy for Brain Health
Theta Burst TMS for Brain Potential & Recovery
Top 4 Autism Treatment via MeRT Therapy