If you’ve ever wondered about TMS therapy and keep seeing terms like TMS vs rTMS, you’re in for clarity through this friendly, thoughtful breakdown. Let’s explore the key differences, why they matter, and how each approach can benefit you.
Understanding the Basics
TMS therapy – The broad concept
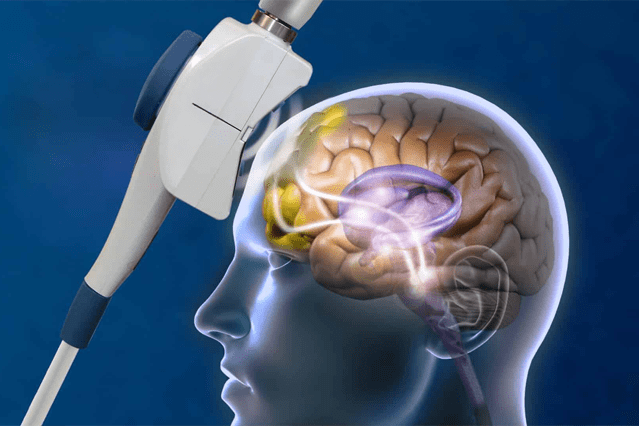
TMS therapy stands for transcranial magnetic stimulation. In simple terms, it’s a noninvasive treatment where magnetic pulses are delivered to specific brain areas to influence neural activity. It’s often used for mood-related conditions when standard approaches don’t work.
rTMS – A focused, repetitive delivery
When you add the “r” to TMS, it stands for repetitive TMS. That’s right, this method involves delivering repeated magnetic pulses in a session, aiming to build more lasting effects in brain circuits.
So in the TMS vs rTMS comparison, TMS therapy is the general technique, while rTMS is its most common form using repeated pulses.
TMS vs rTMS: How Are They Different?
Let’s break down the differences elegantly:
a) What’s actually happening
- TMS therapy refers broadly to the use of magnetic stimulation on the brain.
- rTMS applies that technique in repetitive pulses across sessions to create a cumulative effect.
b) Coil design and depth of stimulation
- rTMS usually uses a figure-8 coil, which targets brain areas close to the surface, about 0.7 to 1 cm deep.
- In contrast, deep TMS (dTMS), a version of TMS therapy, uses an H-coil or similar designs to reach deeper and wider brain regions up to 3–4 cm, though still often counted as within the broader TMS scope.
c) Session duration and treatment schedules
- TMS therapy (especially deep TMS versions) typically features shorter sessions around 20 minutes.
- rTMS sessions last longer, often 30 to 40 minutes or more, depending on the protocol.
When to Use Each One
TMS therapy for broad impact
With its variety of coil types, TMS therapy can be tailored to specific depths or brain zones. Deep versions have approval for conditions like OCD and smoking cessation, along with depression.
rTMS for targeted, repeated practice
Since rTMS delivers focused, repetitive pulses, it’s especially effective in rewiring or rebalancing brain activity in mood-related areas. It’s widely accepted and commonly used for major depression, especially when other treatments haven’t worked.
Similarities Worth Highlighting
Even with the TMS vs rTMS contrast, they share core traits:
- Noninvasive: Both avoid surgery or anesthesia, meaning you can resume normal activity right afterward.
- Well tolerated: Side effects like mild headaches or scalp discomfort are common, but usually temporary.
- Structured schedules: Both usually involve daily sessions over several weeks, often 4 to 6.
- Coverage and access: Many insurance plans now cover treatments under the umbrella of TMS therapy, including rTMS.
The Takeaway: TMS vs rTMS in Real Life
When you’re comparing TMS therapy to rTMS:
- Use TMS therapy when you want flexibility in targeting deeper or broader brain areas. It’s the umbrella term and includes specialized forms like deep TMS.
- Look at rTMS if you’re after a well-studied, repetitive pulse protocol, especially for depression treatment.
Why this matters to you
Understanding TMS vs rTMS helps you talk confidently with your provider and compare available options. Knowing how long sessions take, how deep they penetrate, and which conditions each suits empowers better decisions.
Quick Summary – Your Handy Reference
- TMS therapy is the general term that refers to all types of transcranial magnetic stimulation techniques.
- rTMS means repetitive TMS, where pulses are delivered repeatedly in each session to build a lasting effect.
- Deep TMS (a subtype) makes use of an H-coil that allows stimulation to reach deeper and wider brain regions compared to standard coils.
- Session time varies between the two. rTMS sessions usually take longer, while deep TMS sessions are typically shorter.
- Common uses overlap, as both approaches are widely used for depression. Deep TMS also has approval for conditions such as OCD and smoking cessation.
Final Thoughts
The next time you hear TMS therapy or wrestle with TMS vs rTMS, you’ll know:
- TMS therapy is a broad category of magnetic brain treatment.
- rTMS is the most common, repetitive variant focused on mood circuits.
- Coil design, depth, and session patterns matter for your comfort, effectiveness, and convenience.
By knowing these distinctions, you’re better equipped to ask the right questions, understand treatment options, and feel confident moving forward. Here’s to smart, human-centered learning and making empowered choices in your wellness journey, and now you have the clear, fresh insight into TMS vs rTMS.